In healthcare settings, such as surgery centers and ambulatory care facilities, surgical pathological waste management is critical for ensuring safety and compliance. This waste category includes human or animal tissues, organs, and body parts removed during medical procedures, making its proper disposal essential to prevent infections and environmental harm.
This comprehensive guide highlights what surgical pathological waste entails, its risks, and the best practices for its safe and compliant disposal.
What is Pathological Waste?
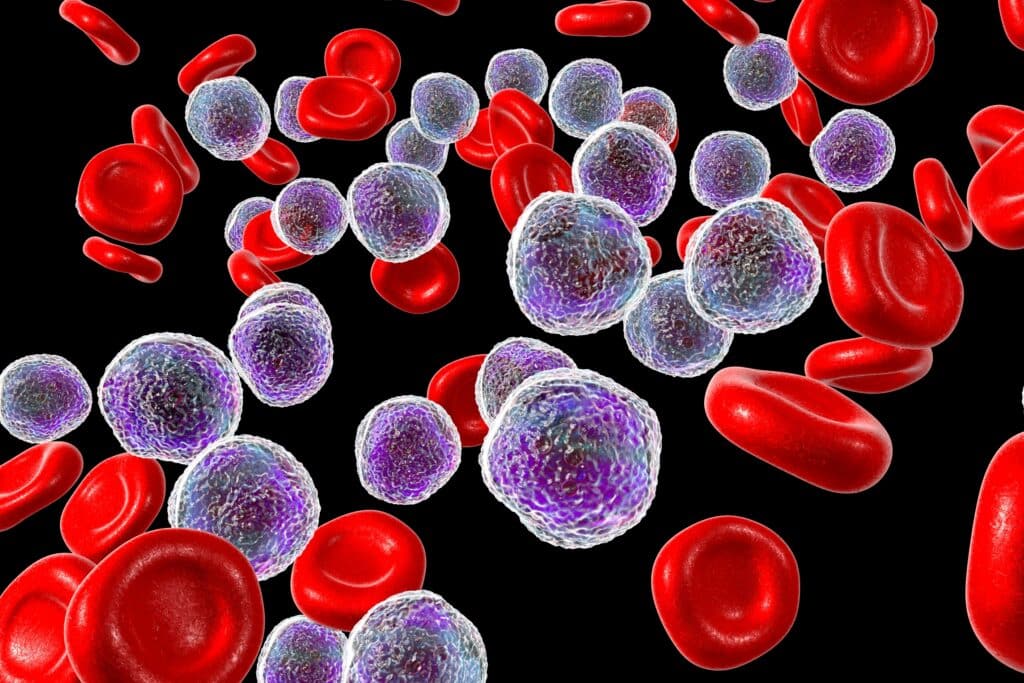
Pathological waste is a specific type of medical waste that comes from surgical procedures and includes things like tissues, organs, and body parts removed during operations. While medical waste is a broader category that covers items like gloves, gauze, and used instruments, pathological waste is more biologically sensitive and carries higher risks if it’s not handled properly. Because of its organic nature, it requires more specialized disposal methods—typically incineration—to completely destroy any potential hazards. For surgery centers, managing pathological waste is especially important due to the volume and type of materials they deal with daily. Getting it right isn’t just about compliance; it’s about protecting the health of patients, staff, and the environment.
Pathological waste is more than just another category of medical waste—it poses unique and significant risks that require careful management. Because it includes human tissues, organs, and other biological materials, this type of waste has a higher potential to spread infectious diseases if mishandled. The organic nature of pathological waste also makes it prone to decomposition, which can release harmful pathogens and create environmental hazards, such as contamination of air, soil, or water. For surgery centers, which generate this waste in large volumes during procedures, proper disposal isn’t just a regulatory requirement—it’s a critical step in preventing the spread of disease, protecting public health, and minimizing environmental damage.
Other Types of Waste in Surgical Centers
Types of Medical Waste in Surgery Centers: A Focus on Pathological Waste
Surgery centers generate various types of medical waste, but pathological waste stands out due to its volume, complexity, and the risks it poses. Proper management of pathological waste is crucial for maintaining safety, compliance, and environmental responsibility. While other types of waste—biohazard, sharps, and pharmaceutical—play a role in waste management protocols, surgical pathological waste requires unique handling and disposal. Below is an overview of these waste types, emphasizing their significance in surgery centers:
1. Surgical Pathological Waste
Surgical pathological waste is a significant byproduct of procedures in surgery centers and includes:
- Excised Tissues and Organs: Removed during biopsies, tumor excisions, or amputations.
- Body Fluids: Collected during surgeries, such as thoracentesis or wound drainage.
- Unused Blood Products: Often discarded after specific types of surgical procedures.
Why It Matters in Surgery Centers:
Pathological waste presents heightened risks due to its biological composition. If mishandled, it can contribute to the spread of infectious diseases and environmental contamination. The organic nature of this waste makes it prone to decomposition, releasing pathogens and harmful gases, which underscores the importance of immediate and secure disposal.
Disposal Requirements for Pathological Waste in Surgery Centers:
- Pathological waste must be segregated at the source and placed in leak-proof, clearly labeled containers.
- If disposal cannot occur immediately, waste should be refrigerated to prevent decomposition.
- Certified medical waste haulers transport this waste for incineration, which ensures complete pathogen destruction and compliance with regulations.
2. Biohazard Waste
While not as biologically complex as pathological waste, biohazard waste in surgery centers still requires careful handling. Examples include:
- Surgical Drapes and Gowns: Contaminated with blood or bodily fluids.
- Wound Dressings and Absorbent Pads: Commonly used during post-operative care.
- Lab Cultures and Specimens: Diagnostic samples collected during surgeries.
Key Difference from Pathological Waste:
Biohazard waste is typically less prone to decomposition but can still harbor infectious agents. Unlike pathological waste, it is usually treated with sterilization methods such as autoclaving.
3. Sharps Waste
Surgery centers generate high volumes of sharps waste due to the precision instruments used in procedures. These include:
- Scalpels and Needles: Integral to surgical operations.
- Broken Glassware: Often from medication vials used during procedures.
Key Difference from Pathological Waste:
While sharps waste poses immediate physical injury risks, pathological waste carries biological risks that demand specialized disposal methods, like incineration.
4. Pharmaceutical Waste
Medications and anesthesia play a vital role in surgical procedures, leading to pharmaceutical waste such as:
- Unused or Expired Medications: Including anesthetics, pain relievers, and antibiotics.
- Contaminated Packaging: Residual IV bags or empty bottles used during surgery.
Key Difference from Pathological Waste:
Pharmaceutical waste is largely an environmental risk if not properly segregated, while pathological waste primarily threatens biological safety and health.
The Importance of Pathological Waste Management
Unlike other waste types, surgical pathological waste requires more stringent protocols due to its higher biological risks. Mismanagement can result in:
- Infectious Disease Spread: Due to the presence of viable pathogens.
- Environmental Damage: From decomposition-related contamination.
- Regulatory Non-Compliance: Leading to hefty fines and legal repercussions.
Proper management of pathological waste not only ensures safety but also reflects the high standards of care surgery centers are expected to maintain.
For more on waste management best practices, explore our Medical Waste Segregation Tips.
Segregate pathological waste from other medical waste for effective management. Labeled containers must be in use. Storage of pathological waste requires a secure area inaccessible to unauthorized personnel and adequate ventilation and temperature control.
Transporting pathological waste to licensed disposal facilities should be handled by authorized medical waste transportation companies. These professionals have the expertise to transport such hazardous materials safely.
Pathological waste undergoes neutralization using incineration, autoclaving, or microwave treatment methods at the disposal facility. These techniques destroy pathogens and reduce the volume of waste, minimizing potential risks associated with its disposal.
Segregation and Disposal of Pathological Waste
Proper disposal of surgical pathological waste starts with segregation at the point of generation. This initial step is critical to maintaining compliance, ensuring safety, and streamlining the waste disposal process in surgery centers.
- Segregation Requirements:
- Dedicated Containers: Pathological waste must be placed in leak-proof, clearly labeled, and puncture-resistant containers specifically designated for this waste type. These containers are usually red or yellow and labeled with a biohazard symbol for easy identification.
- Double Bagging: Use heavy-duty biohazard bags to line the container. Ensure the bags are durable enough to prevent leaks or punctures during handling and transportation.
- Separate from Other Waste: Pathological waste must not be mixed with sharps, general biohazard waste, or pharmaceutical waste to avoid cross-contamination.
- Storage Guidelines:
- Volume Limits: Facilities must adhere to state and local regulations regarding the maximum volume of pathological waste allowed on-site at any given time, which often ranges from 50 to 200 pounds, depending on the facility’s size and location.
- Temperature-Controlled Storage: If immediate disposal is not possible, pathological waste must be stored in a refrigerated or frozen environment (typically below 7°C or 45°F) to prevent decomposition and the release of odors or pathogens.
- Time Limits: Most regulations require that pathological waste be disposed of within seven days if stored at room temperature or 30 days if refrigerated or frozen.
- Documentation and Tracking:
- Facilities must maintain detailed logs, including the type and volume of waste, storage duration, and disposal records, to comply with OSHA, EPA, and state regulations.
Once properly segregated and stored, surgical pathological waste is treated using specialized methods designed to neutralize pathogens and minimize environmental impact.
1. Incineration
Incineration is the gold standard for disposing of surgical pathological waste due to its effectiveness and compliance with stringent regulations.
- Process:
- Waste is transported to a licensed incineration facility.
- At temperatures exceeding 850°C, organic materials are combusted into sterile ash.
- Emissions are filtered through scrubbers to reduce environmental pollutants.
- Advantages:
- Eliminates all biological hazards, including prions and viruses.
- Reduces waste volume significantly, often by 90% or more.
- Compliant with most state and federal requirements for pathological waste.
- Considerations:
- Facilities must ensure they use certified haulers and incinerators to meet regulatory standards.
- High energy usage can increase disposal costs.
2. Autoclaving
Autoclaving, or steam sterilization, is suitable for smaller amounts of pathological waste, particularly tissues and fluids that do not require incineration.
- Process:
- Waste is loaded into an autoclave and exposed to high-pressure steam at 121°C to 134°C for a specified duration.
- Pathogens are destroyed through heat and moisture exposure.
- Advantages:
- Environmentally friendly, producing no harmful emissions.
- Cost-effective for facilities generating small amounts of surgical pathological waste.
- Considerations:
- Not effective for large body parts or high-moisture tissues.
- Requires waste to be shredded or resized before treatment.
3. Microwave Treatment
Microwave treatment is an emerging option for facilities seeking sustainable disposal methods.
- Process:
- Waste is shredded and placed into a microwave unit.
- High-frequency waves heat the waste to destroy pathogens, leaving sterilized, non-hazardous material.
- Advantages:
- Reduces waste volume while maintaining environmental integrity.
- Can be performed on-site, minimizing transportation needs.
- Considerations:
- Limited to small waste volumes and facilities with appropriate equipment.
- Initial investment costs for microwave systems are high.
Regulations
- Volume and Storage Compliance: Surgery centers must follow specific guidelines for how much pathological waste can be stored on-site and for how long. Failure to comply can result in hefty fines or operational disruptions.
- Licensed Transportation: Only certified medical waste haulers can transport pathological waste to disposal facilities.
- Documentation: Facilities must keep detailed manifests of waste pickups, transportation, and treatment to demonstrate compliance.
Why Proper Handling and Disposal Matters
Mishandling surgical pathological waste can lead to serious risks, including:
- Infectious Disease Outbreaks: Pathogens in decomposing tissues can spread through contact or airborne particles.
- Environmental Contamination: Improper storage or disposal can lead to leaching of hazardous materials into soil or water.
- Regulatory Penalties: Non-compliance with EPA, OSHA, and local regulations can result in fines and reputational damage.
For further information on safe and compliant disposal practices, visit the EPA’s Medical Waste Management page.
MedPro Disposal: Your Partner in Medical Waste Disposal
At MedPro Disposal, we make managing surgical pathological waste straightforward and stress-free, so you can focus on what matters most—your patients. Our tailored solutions prioritize your facility’s safety, compliance, and budget, delivering unmatched value every step of the way.
Here’s how we support your success:
- Enhanced Safety and Compliance: Stay worry-free knowing we adhere to all regulatory standards, keeping your facility protected and compliant.
- Environmentally Responsible Practices: Partner with a team committed to reducing environmental impact with every disposal.
- Transparent, Cost-Effective Solutions: Enjoy straightforward pricing without hidden fees, helping you plan with confidence.
From seamless waste segregation to secure transportation and disposal, MedPro Disposal ensures every detail is handled with care and precision. Discover how we can simplify your waste management needs and elevate your facility’s operations by exploring our waste disposal services.